Urinary tract infections (UTIs) are more prevalent in women than men because women have a shorter urethra, allowing bacteria to enter the urinary tract more easily. The urethral opening in women is also close to the anus and vagina, which can be sources of bacteria.
Studies show that 50%–60% of women experience a UTI at least once in their lifetime.(1) Hormonal fluctuations and other changes in the body during menopause may further elevate this risk.
Knowing the common causes and symptoms of UTIs can help women take precautions to prevent them or seek medical help when the condition becomes recurrent or severe.
What are urinary tract infections?
UTIs are bacterial infections in the urinary system, which consists of the urethra, ureters, bladder, and kidneys. Bacteria entering the urethra can cause infections in any part of the urinary system, particularly in the bladder.(1)
A recurrent UTI is when three or more medically diagnosed UTIs occur within a year, with each infection being completely treated before the next one starts.(1)
A 2019 study reveals that 19%–36% of premenopausal women experience recurrent UTIs, and the recurrence rate significantly increases to 55% after menopause.(2)
Why are UTIs more common during menopause?
Menopause can cause the following changes in the vagina and urinary system that may increase the risk of UTI:(2,3)
Altered Urogenital Microbiome
The journal of the International Menopause Society suggests that estrogen can influence the composition of the urogenital microbiome, which consists of healthy bacteria in the vagina and urinary system. These bacteria serve as a natural defense against harmful bacteria that can cause UTIs.
Before menopause, the vagina is typically home to a type of bacteria called Lactobacillus. The vaginal wall produces glycogen, a type of glucose, which is fermented by Lactobacillus to create lactic acid. This process maintains the pH of the vagina and prevents other types of bacteria from entering. As estrogen level declines during menopause, the vaginal pH may increase with a drop in Lactobacillus bacteria, which might make the vagina vulnerable to infection.
Genitourinary Syndrome of Menopause (GSM)
GSM is an umbrella term for changes in the urogenital system, including vulvovaginal atrophy, atrophic vaginitis, and urinary incontinence. The urogenital system has estrogen receptors that help keep the organs elastic and moist.
Estrogen loss can weaken the muscles of the urethra, making it easier for harmful bacteria to enter the urinary tract and reach the bladder. GSM can also alter the lining of the urogenital system, leading to a decrease in glycogen production, which can compromise the natural defense against UTI-causing bacteria.
Low estrogen levels may also weaken the pelvic floor muscles and cause incomplete bladder emptying, allowing bacteria to linger and multiply.
Certain Diseases
Declining estrogen levels during menopause may cause certain health conditions, such as diabetes and urinary incontinence, which can contribute to UTIs.
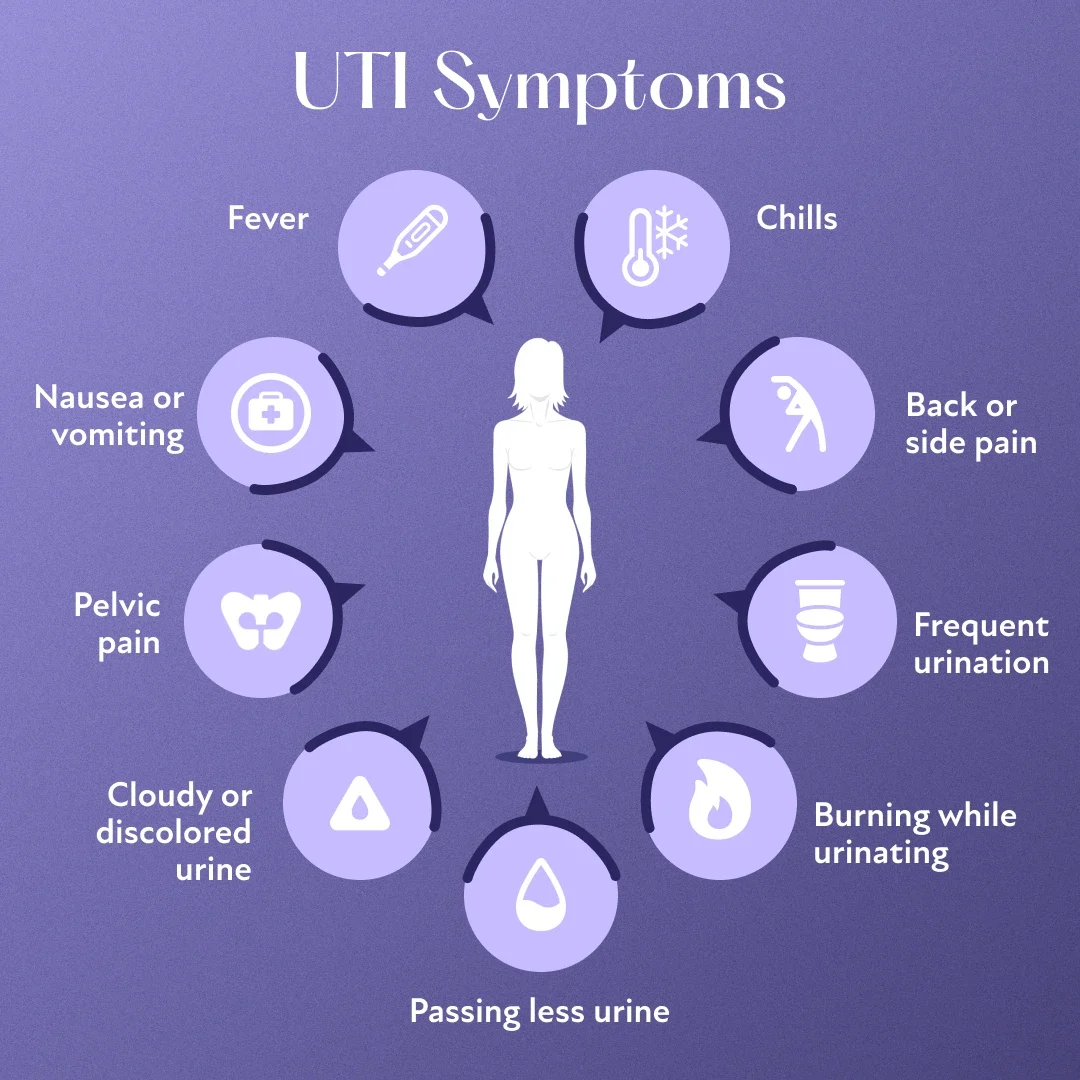
Urinary Tract Infection Symptoms During Menopause
Some common symptoms that may indicate a UTI include the following:
Burning sensation during urination
Frequent urination
Cloudy, bloody, or strong-smelling urine
Pelvic pain during intercourse
A feeling that the bladder hasn’t been fully emptied
Fever
Higher resting heart rate
Pain in the lower back
How to Prevent UTIs During Menopause
Preventing recurrent UTIs is a crucial aspect of care for postmenopausal women. The following approaches can help reduce the risk of UTIs:
Managing the Underlying Cause
The reason for recurrent UTIs can vary among individuals. GSM may be a contributing factor for some women, while sexual transmission might be the cause for others. Consulting a physician can help identify the underlying issue and find the best ways to manage or prevent these infections.
Improving Urination Habits and Hygiene
This is one of the most effective actions that can help reduce the frequency of UTIs or even prevent their recurrence. Some changes in urination habits that might help include the following:
Sitting comfortably on the toilet seat and not squatting
Relaxing the pelvic floor muscles when urinating
Allowing enough time to fully empty the bladder
Emptying the bladder after sex to flush away any bacteria that may have entered the urinary tract
Using sanitary pads in place of tampons and changing pads each time one uses the bathroom
Avoiding the use of feminine hygiene products, bath oils, or douches
Wiping from front to back after using the bathroom
Cleaning the anal and genital areas before and after sex
Considering Prophylactic (Preventive) Antibiotics
Some women might benefit from taking low-dose probiotics daily or after sex. Studies reveal that post-coital antibiotics can reduce the frequency of sex-related UTIs. However, because misuse of these antibiotics can lead to resistance, they should only be taken after consulting a physician.(2)
Using Vaginal Estrogen
Vaginal estrogen is available in various forms, including rings, tablets, and creams. It supplies estrogen locally and can help support the health of vaginal flora.
A 2019 article suggests that vaginal estrogen might restore Lactobacillus within three months of use and improve defense against harmful bacteria.(2)
Trying Non-Medicinal Approach
Effective non-medicinal options include the following:(2,4)
D-Mannose: This over-the-counter monosaccharide sugar may help prevent bacteria from attaching to the vaginal or urinary bladder wall. D-mannose may be as effective as nitrofurantoin, a commonly used antibiotic for managing UTIs.
Methenamine salts: These are considered to have antibacterial properties.
Cranberry products: Various studies indicate that cranberry products might help prevent recurrent UTIs. However, there isn't enough evidence to fully support this benefit.
Treatments for Recurrent UTIs in Postmenopausal Women
Effective approaches for reducing the risk of UTIs during menopause include topical estrogen, antibiotics, and symptomatic management.
Topical Estrogen
Vaginal estrogen is one of the most viable options for reducing the risk of UTIs during menopause. It raises estrogen levels, which promotes the elasticity of the genitourinary system and supports a healthy bacterial count. Experts believe that vaginal estrogen may be more effective than oral estrogen in managing UTIs during menopause.
Antibiotics
A physician can help determine the appropriate antibiotic based on the symptoms and/or urine culture results. Commonly prescribed antibiotics include nitrofurantoin and sulfamethoxazole.
Individuals should always consult a physician before taking antibiotics, as inappropriate use can lead to antibiotic resistance. It also helps to start treatment as early as possible to prevent the risk of UTI-related complications, such as bladder inflammation.
Symptomatic Relief
Adequate hydration is key to flushing out bacteria through urine. A physician might also recommend pain relievers or non-steroidal anti-inflammatory drugs to manage pain or discomfort associated with UTIs.
Menopause & UTIs: Leading a Comfortable Life
By understanding the risk factors and taking preventive measures, women can significantly reduce their chances of developing UTIs during menopause. Early diagnosis and treatment are crucial if a UTI occurs. It’s recommended to consult a doctor about any concerns related to UTIs. They can provide guidance on treatment approaches to ensure a smoother transition through menopause and minimize the risk of complications.
When should individuals seek medical attention for a UTI?
Anyone experiencing a severe or recurrent UTI should consult a physician. Some symptoms that might indicate a severe infection include the following:(5)
Blood or pus in urine
Burning pain while passing urine
Increased frequency of urination
Worsening fever, chills, or nausea
Pain in the back below the ribcage
Experiencing UTIs during menopause? Discover if HRT is right for you.
If you’ve entered the menopause transition and are struggling with UTIs, you don’t have to suffer in silence. Take our brief menopause quiz to see if you’re an eligible candidate for HRT. Get started with Winona to take the first step toward feeling better.
