If you’re in your late 30s or mid-40s and still getting periods, but new and confusing symptoms have you feeling like a stranger in your own body, you’re not imagining it — it’s likely perimenopause.
Perimenopause is the transitional stage before menopause when your hormone levels begin to shift and change. These fluctuations affect nearly all parts of the body, causing symptoms that may feel strange or uncomfortable. Symptoms can last for years and are a normal part of the menopausal transition. However, just because it’s normal, it doesn’t mean you should have to spend years of your life in discomfort.
If you’re tired of conflicting online information or frustrated that your doctor isn’t taking your symptoms seriously, consider this your personal, evidence-based resource for what to expect. Learn to identify the first signs of perimenopause and gain strategies and treatment options to manage hormonal ups and downs, so you can finally feel like yourself again.
Understanding Perimenopause: The Transition Before Menopause
Perimenopause is the first stage of the menopausal transition.(1) Understanding what’s going on inside of your body and how to tell the difference between menopause and perimenopause can help you feel less anxious about navigating the transition.

The “On-Ramp” to Menopause
If menopause were a highway, perimenopause would be considered the “on-ramp.” Perimenopause refers to the years leading up to your final menstrual period (FMP), when your body is going through significant hormonal changes, but you’re still getting periods.(1)
These hormonal shifts affect many different parts of your body, including the bones, tissues, and muscles. These changes also alter how your body regulates mood, sleep, digestion, and temperature, causing a wide range of physical and emotional symptoms.
The Hormonal Rollercoaster (Not a Gentle Decline)
Estrogen is the primary sex steroid hormone in your body. It supports the development of your reproductive system and regulates your monthly menstrual cycle. Progesterone’s job is to get the uterus ready for a potential pregnancy after ovulation, while testosterone helps regulate your sex drive.(2)(3)

During the postmenopause stage, hormone levels steadily decline and stay at a new low for the rest of women’s lives. Perimenopause is the opposite experience; levels of estrogen, progesterone, and testosterone rise and fall unpredictably during this stage. This happens because your ovaries have a limited number of eggs during your lifetime. As women age, the supply of eggs decreases and the ovaries begin to produce less estrogen and progesterone.(4)
The Key Difference Between Perimenopause and Menopause
The key difference between perimenopause and menopause is that women still get periods during the perimenopause stage. Menopause, on the other hand, is the point after which periods have stopped completely. Menopause is confirmed once you’ve gone 12 months in a row without menstruating.(5)
Your periods will become irregular during perimenopause, but because you’re still menstruating, it’s possible to become pregnant. Therefore, it’s recommended that women continue to use birth control until age 50 for pregnancy prevention.
Common Signs & Symptoms of Perimenopause
Each woman’s personal experience of the menopausal transition will vary. However, below you’ll find some of the most common signs of perimenopause, including which symptoms you might notice first.
Change #1: Your Menstrual Cycle Becomes Unpredictable

Irregular periods are usually the first sign of perimenopause. These changes may seem concerning at first, but they are a completely normal part of the transition.
Your periods may last longer or shorter than usual, and the flow may become lighter or heavier. You may also begin to miss periods, which is common during the early perimenopause stage.
As you move into the late perimenopause stage, you’ll notice your cycles becoming even more unpredictable. It’s not unusual to go anywhere from 60 days to several months between periods.(1)
Change #2: Your PMS Gets Worse

Cramping, bloating, mood changes, and other symptoms of premenstrual syndrome (PMS) may get worse during perimenopause if you’re naturally sensitive to hormonal shifts. The reason you may experience worsening PMS symptoms during this stage of life is likely due to fluctuating hormone levels that can impact many of the body’s systems.(6)
Estrogen and progesterone are believed to affect mood-regulating hormones. Changes in pain perception have also been linked with shifting levels of estrogen and progesterone, particularly during different phases of the menstrual cycle, which may have a similar effect during perimenopause.(7) These factors may contribute to heightened emotional symptoms during the menopausal transition.
Hormonal fluctuations can also change the speed at which food moves through the gut, potentially influencing worsening gastrointestinal symptoms, such as those often associated with PMS.(7)
“I used to suffer from PMS for 3 to 4 weeks out of the month and I was at my wits end. I found Winona and I’m so grateful that I did because now my PMS symptoms last 3 to 7 days out of the month and it’s not nearly as severe. Thank you Winona!” –Winona patient
Change #3: New Mood & Sleep Challenges Appear

Hormonal changes can cause significant mood disruptions during perimenopause. You may feel fine one moment, only to feel upset or irritated a little while later. It’s also common for women to experience anxiety during these transitional years. This is because estrogen influences signaling pathways of neurotransmitters like serotonin and norepinephrine, which are both involved in regulating your mood.
Struggling to fall asleep or waking up drenched in the middle of the night from night sweats? Hormonal changes can be the cause of sleep challenges too. Approximately 40% of women are affected by sleep problems during the menopause transition, including sleep disorders like insomnia.(8) Along with mood changes and vasomotor symptoms, drops in progesterone — a calming hormone — may also contribute to sleep disruptions during perimenopause.(9)
Change #4: Early Physical Symptoms Emerge

Some of the most common early physical symptoms of perimenopause are hot flashes, night sweats, and vaginal dryness.
Vasomotor symptoms (hot flashes, night sweats) are a result of hormonal changes that throw off your body’s internal thermostat. Hot flashes are sudden sensations of heat felt in the face and upper body. You may also sweat or your skin may flush. They typically come and go within 5 minutes. However, just because they may be short-lived, doesn’t mean they aren’t disruptive to women’s daily lives. As many as 74% of perimenopausal women experience hot flashes.(10)
Many women also grapple with night sweats as they enter the menopausal transition.
Vaginal dryness is another signature early sign of perimenopause. When estrogen levels drop, the vaginal tissues become thin and dry. This can lead to irritation, burning sensations, painful sex, or a dip in your sex drive.(1)
The Perimenopause Timeline: When does it start and how long does it last?
There is no definitive timeline for perimenopause. It lasts an average of four years, although some women may spend anywhere from five to ten years in this transitional stage.(1)(11)

The average age women enter perimenopause is 47, although it can start earlier or later.(11)(12) If you’re under 45 and have started noticing symptoms, you might be wondering, “Am I too young for this?” Not necessarily — it’s possible for perimenopausal symptoms to set in during your early 40s or even your late 30s.(1)
Researchers from a study of over 4,000 women in the United States (U.S.) found that about 21% had reached out to a doctor about perimenopausal or menopausal symptoms. Nearly one-third of these women were between the ages of 30 and 45. After consulting with a healthcare provider, over 25% of the women aged 30 to 35 were diagnosed perimenopausal, along with 40% of those aged 36 to 40.(1)
If you reach menopause before the age of 45, it’s defined as early menopause. If menopause occurs before age 40, it’s known as premature menopause. Approximately three in every 100 women will experience premature menopause. The cause isn’t always known, but genetics, health conditions, or certain surgeries can play a role.(13)(14)

It’s understandable that perimenopausal symptoms that come on at an earlier age may cause some women to worry. Consulting with a knowledgeable physician helps ensure your questions are answered and that you receive timely treatment and ongoing support for your long-term health.
How Perimenopause Is Diagnosed
There is no diagnostic test that can determine whether you’ve started the menopausal transition. Instead, your doctor will consider your age, health history, and any medications you’re taking. However, your symptoms are the most important diagnostic tool.

Why Your Symptoms Are the Most Important Clue
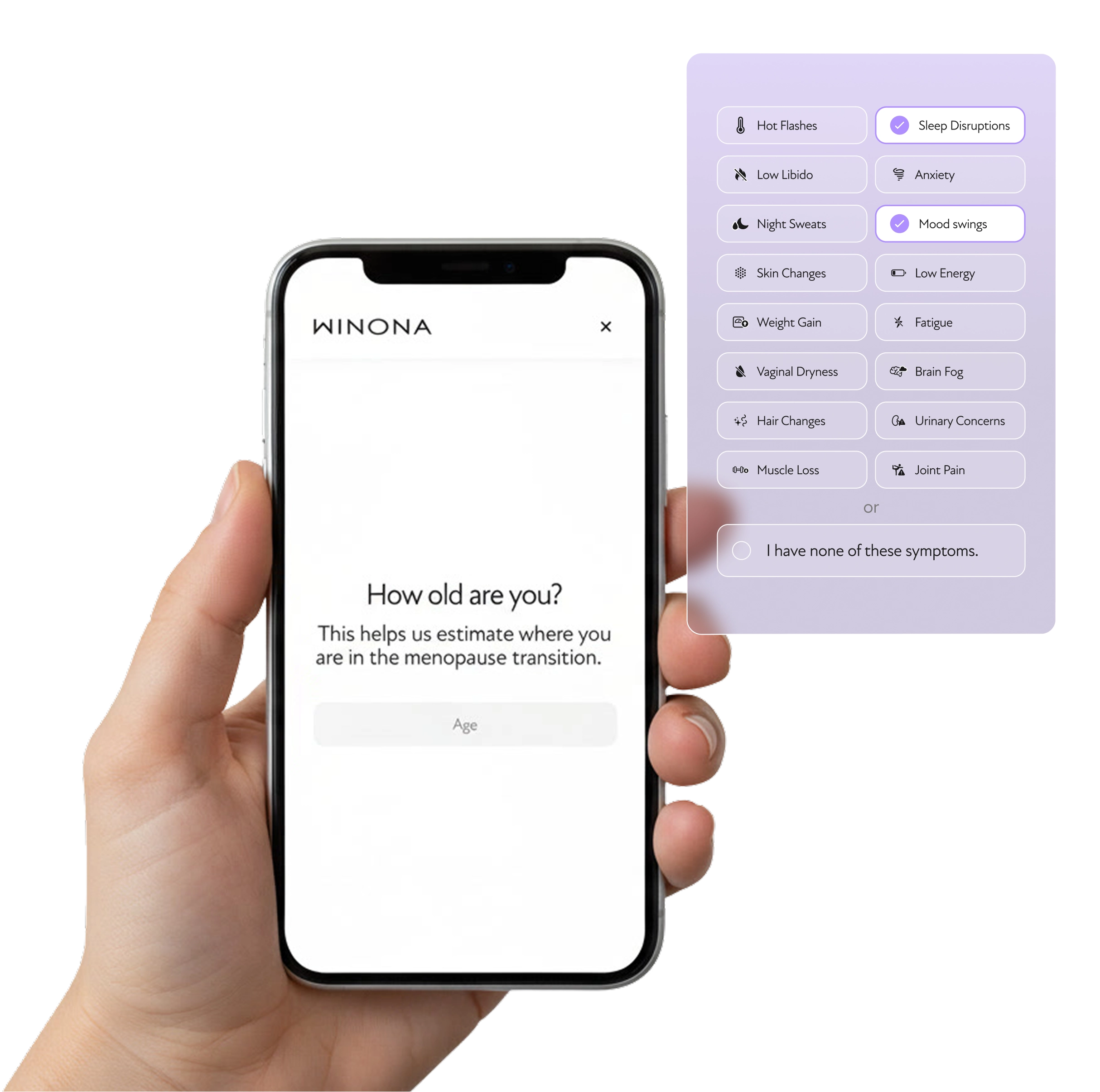
You know your body best, so what matters most is your personal description of your symptoms. While there are over 100 symptoms of perimenopause, hot flashes, night sweats, mood changes, and vaginal dryness are some of the key signs that signal to your doctor you’re likely in the menopausal transition.
One of the best ways you can provide your clinician with the most information is by logging your symptoms in a menopause symptom tracker. The more details you share, the more your doctor can get a better sense of what’s happening. Write down what the symptom is, how long it usually lasts, how intense it feels, and how often it’s happening.
The Problem with Hormone Testing in Perimenopause
Hormone tests are used to detect hormonal imbalances in the body. Therefore, it’s logical to think that they could help determine if a woman is perimenopausal — but hormone testing isn’t necessary to diagnose perimenopause.(15)
The problem is that hormone tests often paint an incomplete picture of what’s going on inside your body. Hormone levels change on a daily basis. A single test will only reveal what your hormones were doing at the time the test was taken, rather than showing your doctor what’s happening overall.
While hormone testing can be helpful in diagnosing certain medical conditions, they are not a reliable means of determining a woman’s menopause status.
The Best Next Step: Talk to a Specialist
If perimenopausal symptoms are impacting your day-to-day life, the next best step is to talk with a provider who can validate your experience and specializes in working with perimenopausal women. Consulting a specialist helps you receive treatment sooner rather than later. It’s also important to rule out any other health issues that may be causing your symptoms.
Treatment and Relief for Perimenopause Symptoms
You don’t have to live with the discomfort of perimenopause for years on end. A combination of lifestyle changes and hormonal treatment options can help make your body feel like yours again.
Lifestyle Support for Symptom Relief
The following lifestyle changes can help in managing perimenopausal symptoms:(16)(17)
Creating a Relaxing Bedroom Environment:
If anxiety or night sweats are preventing you from getting a good night’s sleep, try lowering the thermostat, using cooling pillows and sheets, or taking a cool shower before climbing into bed.
To signal to the body that it’s time for sleep, avoid using electronics in the hours before bed. Instead, try easing into sleep with mind-body practices like progressive muscle relaxation, a technique that has been shown to improve sleep quality and daytime fatigue among postmenopausal women.(18)

Getting Regular Exercise:
It’s recommended that adults get 150 minutes (2.5 hours) or more of moderate-intensity exercise on a weekly basis. It’s also recommended to work in two days of muscle-strengthening exercises.(19)
Weight-bearing activities are particularly important during perimenopause, but they don’t have to be strenuous. Fun activities like walking or dancing also count. Not only may staying physically active help reduce perimenopausal symptoms, it can also prevent long-term health problems.

Maintaining a Healthy Diet:
Making certain dietary changes may help reduce health risks associated with perimenopause, such as bone loss, decreases in lean body mass, and heart disease.
Eating more whole grains, vegetables, fruits, and nuts can give the body the essential vitamins and minerals it needs. Protein is also key during perimenopause, as women require more protein with age. Poultry, fish, and plant sources are ideal options.(20)(21)

Avoiding Hot Flash Triggers:
Caffeine, alcohol, and spicy foods may trigger hot flashes. Keeping intake low may offer some relief.

Wearing Light Clothing to Keep Cool:
Natural fabrics like cotton, linen, silk, bamboo, or hemp will keep you cooler than synthetic fabrics. Mesh and rayon are also breathable materials that won’t trap in heat.

Drinking Enough Water:
Women are recommended to get a total of approximately 11.5 cups of water daily from beverages and foods.(22) Not only is it important to stay hydrated throughout the day, but drinking a little bit of cold water before bed may help prevent night sweats.

Managing Stress Levels:
Some research suggests that yoga, mindfulness meditation, or other stress-reduction activities may reduce or help women cope with perimenopausal symptoms like hot flashes and anxiety.(23)

Avoiding Smoking:
A study showed that women between the ages of 45 and 54 who quit smoking had a lower risk of hot flashes than perimenopausal women who continued to smoke during this stage of life.(24)

Seeking Emotional Support:
It’s critical that women receive emotional support during this overwhelming time, whether from loved ones or a mental health professional. Surrounding yourself with a community of women who can relate to what you’re going through, such as through a support group, can also help you feel less alone.

Hormonal Treatment Options
While lifestyle strategies can offer complementary support, the following hormonal therapies are possible treatment methods for perimenopausal symptoms:

Hormone Replacement Therapy (HRT): HRT, or hormone therapy for menopause, stabilizes the hormonal rollercoaster by increasing levels of estrogen and progesterone that progressively decline throughout the menopausal transition. It’s recognized as the most effective treatment for hot flashes, night sweats, and vaginal symptoms. It’s possible you may notice improvement within just a few weeks of starting treatment, although it can take up to three months to experience the full benefits.(25)(26)
Winona uses bioidentical hormones, which are molecularly identical to your natural hormones. Compared to synthetic hormones, bioidentical hormones are more compatible with the body, which may lead to fewer adverse effects.
A variety of dosing methods exist, allowing you to choose the form of HRT that best fits your lifestyle and individual symptoms. This includes convenient tablets, capsules, patches, body creams, and vaginal creams depending on whether you’re dealing with whole-body symptoms or wanting to specifically target localized symptoms.
Low-Dose Hormonal Birth Control: Combined oral birth control pills with estrogen and progestin may help relieve some symptoms of perimenopause, particularly irregular periods. This is because they contain similar types of hormones as HT for menopause. For women who are still getting periods, low-dose birth control can be a more effective option for regulating the menstrual cycle. However, birth control’s main job is pregnancy prevention, not symptom relief.(27)